Vision MD — Your Specialists for Ocular Diseases
Our vision is essential to every aspect of our lives. That’s why it’s important to make sure our eyes are in good health.
Many of the most common eye conditions and diseases show little or no symptoms at all. That’s why it’s so important, especially as we age, to book regular visits with an eye care professional.
HOW THE EYE WORKS
Your eyes are at work from the moment you wake up to the moment you go to bed. Yet we rarely think about how our eyes actually work. When you take a closer look at all the parts needed for you to see, you’ll start to realize how amazing the visual system truly is.
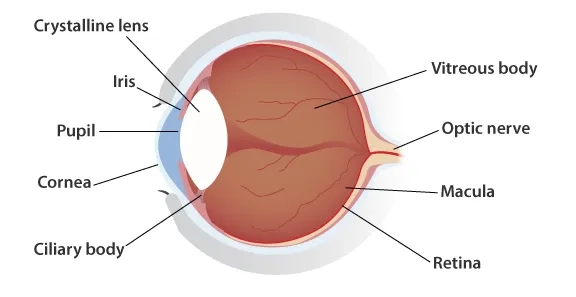
So how does the eye work? The eye is like a camera in the way it captures and focuses the light. Light enters the eye through the cornea, the clear, dome-shaped surface that covers the front of the eye.
From the cornea, the light passes through the pupil. The amount of light passing through is regulated by the iris. The aperture of a camera works in much the same way. From there, the light then hits the lens, the transparent structure inside the eye, which focuses light rays onto the retina.Finally, it reaches the retina, the light-sensitive nerve layer that lines the back of the eye, where the image appears inverted. The retina acts like the film would with a camera.
The optic nerve carries signals of light, dark, and colors to the visual cortex located in our brain. These signals are then assembled into images, which is how we see the world.
COMMON SYMPTOMS
This short guide to common eye symptoms aims to help you learn more about common eye problems or disorders, their symptoms, and—more importantly—how to deal with them.
Since many eye diseases have no early symptoms, are painless, and cause no change in vision, the single best way to protect your vision is through regular professional eye examinations.
Please note that the information contained here should NOT be used as a substitute for the advice of an appropriately qualified and licensed eye care provider. If in doubt, please visit your eye care professional.
EYE PROBLEMS
Common eye problems can be divided into three very broad categories:
- Refractive errors, or problems related to vision
- Eye disorders, or mild annoyances that are usually short-term but sometimes can lead to long-term vision impairment
- Eye diseases, or conditions that warrant a visit to your eye care professional
Since diseases that damage the retina, the optic nerve, or the blood vessels that feed them often cause no pain at all, the single best way to protect your vision is through regular professional eye examinations.
REFRACTIVE ERRORS
The most common vision problems are refractive errors – such as nearsightedness, farsightedness, astigmatism and presbyopia.
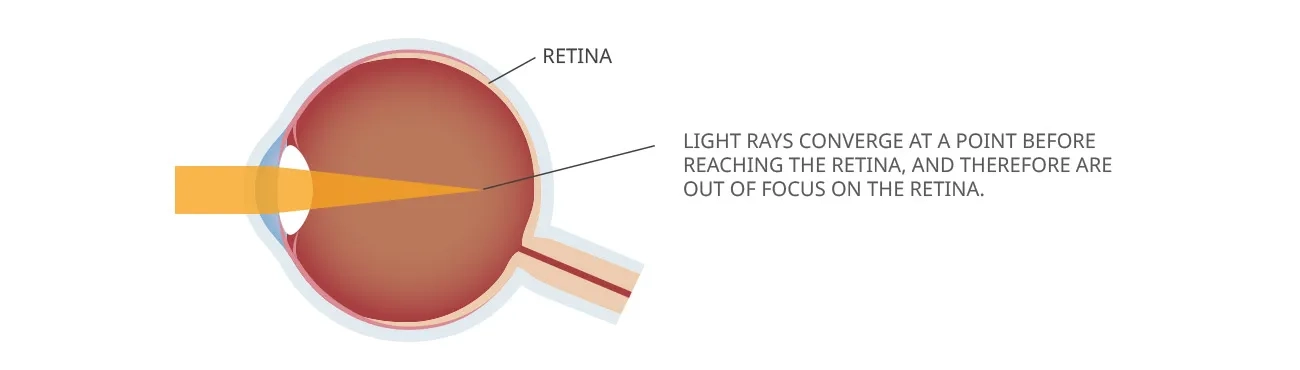
Nearsightedness, or myopia, is a condition in which close objects are usually seen clearly, but objects farther away appear blurred. Nearsightedness occurs when your cornea is curved too much or when your eye is longer than normal. Glasses, contact lenses, and laser vision correction are the most common ways to correct nearsightedness.
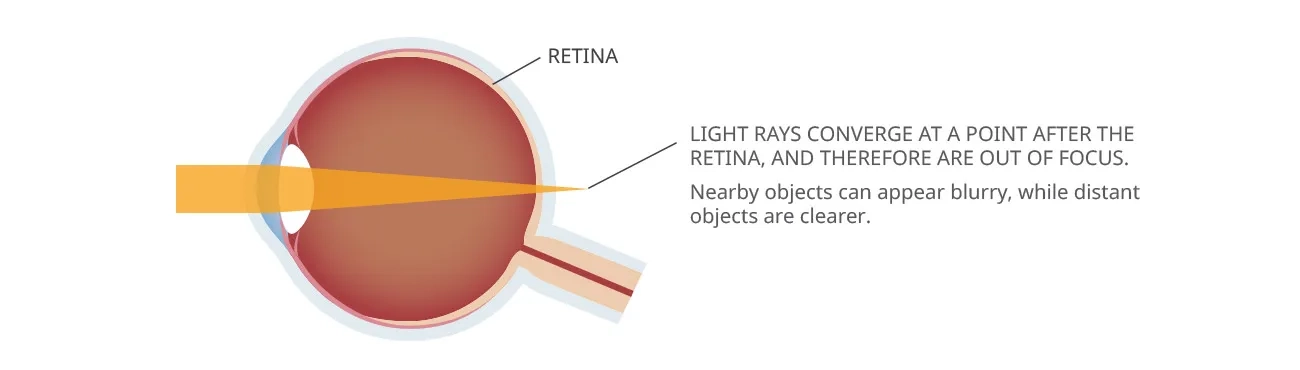
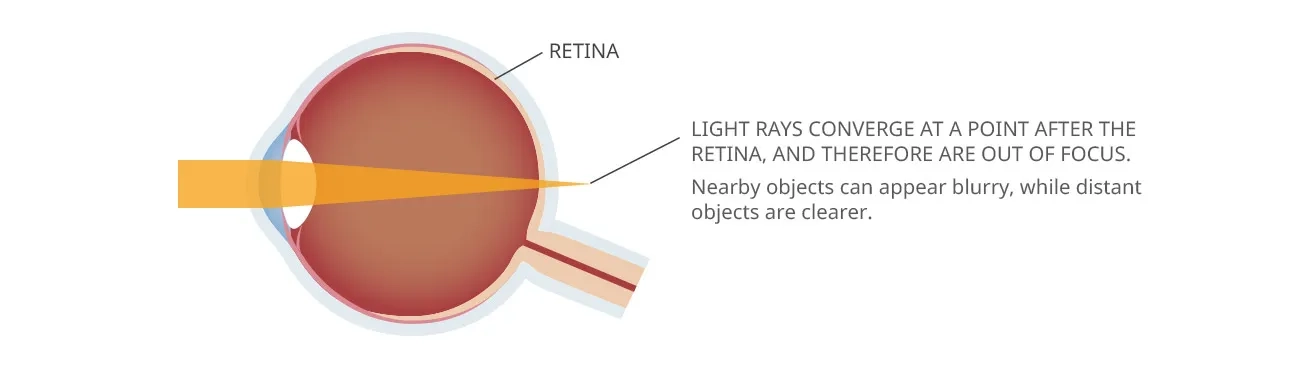
Farsightedness, or hyperopia, is a condition in which distant objects are usually seen clearly, but close ones are not. Farsightedness occurs if your eyeball is too short or the cornea has too little curvature. Your eye care professional can recommend eyeglasses, contact lenses or laser vision correction to correct farsightedness
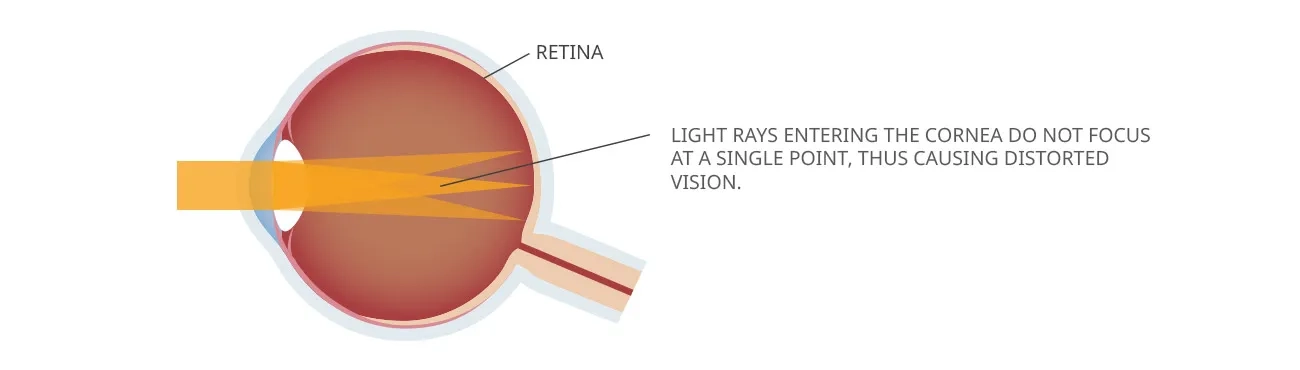
Astigmatism is a common imperfection in the curvature of your cornea and often accompanies nearsightedness or farsightedness. Blurred vision is its main symptom. Astigmatism stems from Eyeglasses, contact lenses, or laser vision correction can correct Astigmatism.
Presbyopia is a normal age-related condition in which your eye’s crystalline lens gradually loses its ability to change shape, making it harder to see objects that are near. Presbyopia can also be corrected by eyeglasses, contact lenses, or surgery.
EYE DISORDERS
Typical eye disorders can be broken down according to their symptoms. Frequent eye symptoms include:
Eye Twitching
Eye twitching, or myokymia, is a widespread complaint. In most cases, only the lower eyelid will be involved. But sometimes the upper eyelid will also act up. These rippling muscle contractions can last days, weeks, and even months before disappearing spontaneously. Frequent contributing factors that trigger twitching are high levels of anxiety, fatigue, overexposure to computer/television monitors, caffeine, alcohol, lack of sleep, and allergies. Eyelid twitching is sometime caused by serious neurological conditions such as blepharospasm and hemifacial spasm. These conditions are however very rare and can sometimes be treated with Botox injections.
Contact your eye care professional if the fluttering persists, causes your eyelid to stay closed, involves other parts of your face, or is accompanied by redness, swelling, or discharge.
Eye Infections
Eye infections are caused by allergies, bacteria, fungus, viruses and other microbial agents. They can also occur after a minor eye injury or a scratch on the cornea. The most common bacterial and viral causes of eye infections are:
- Conjunctivitis – also called “pink eye”
- Bacterial corneal infection - also known as keratitis. It is generally caused by two types of bacteria present in our body, the streptococcus and the staphylococcus
- Blepharitis – is an inflammation of the eyelash follicles. It’s sometimes associated with a bacterial eye infection. Blepharitis can be difficult to manage because it’s often chronic
Eye infections can quickly take a bad turn if left untreated.
The most common complication is corneal ulcers. Ulcers can create a pocket of secretions behind the eye as well as other types of damage that can lead to severe pain and even permanent vision loss. Here are some symptoms which could suggest that you’re suffering from an eye infection:
- Eye pain
- Blurred vision
- A persistent feeling that something is in your eye (foreign body sensation)
- Painful oversensitivity to light (photophobia)
- Yellow, green, bloody, creamy or watery discharge from the eye
- Increasing redness of the eye or eyelids
- A gray or white sore on the coloured part of the eye (iris)
- Fever with no other cause
- Crusting over of the eyelids
If you experience any of these symptoms, call an eye care professional immediately. An eye care professional will give you antibiotic drops when the cause of the infection is not known. Corticosteroid drops may also be used to reduce swelling and inflammation. Other types of drops are also prescribed. Severe ulcers can require a corneal transplant.
If diagnosed and treated early, an eye infection can easily be treated. If no intervention takes place the infection can have devastating consequences, including damage to the retina and the formation of scar tissue and ulcers in the cornea, both of which can have a negative and long-lasting impact on your sight.
Eye Floaters - Eye Flashes
Flashes, also known as photopsia, and floaters are a common, and often benign, eye disorder.
- Eye Flashes:
- Eye Flashes are best described as the sensation of having seen a flash of light or feeling like a light bulb has just flashed on and off in the corner of your eyes. The most common cause is an improper stimulation of the retina, or the optic nerve, which the brain interprets as lights. In some very rare cases, photopsia can be a symptom of retinal detachment or tumours in the eye.
- Floater:
- Floaters, also called spots, are tiny spots or specks that float across the field of vision. In reality, these semi-transparent or cloudy specks are tiny particles moving around within the vitreous, which is the clear, jelly-like fluid that fills the inside of your eyes. Eye Floaters are nothing to worry about unless they are accompanied by eye flashes. The presence of these two eye disorders can indicate a more serious problem such as retinal detachment.
A sudden change in the type and number of spots or flashes you see is also a signal to visit your eye care specialist as soon as possible. By looking in your eyes with special instruments, your eye care professional can determine if what you are seeing is harmless or symptoms of a more serious problem that requires attention.
Eye Strain - Tired Eyes
Eye strain, or tired eyes, is rarely a serious condition.
Associated symptoms can include:
- Tired, itching, and burning eyes
- Difficulty focusing
- Dry or watery eyes
- Blurred or double vision
- Increased sensitivity to light
- Headache or brow-ache
Eye strain is usually caused by activities that require intense use of your eyes for an extended period like:
- Reading
- Writing
- Driving
The use of digital devices is also creating more and more strain on your eyes. Research has shown that users blink less often while in front of a computer screen. This results in drier eyes that burn, itch, and are even more tired.
Eye strain can sometimes be a symptom of an underlying medical condition requiring professional intervention. If eye fatigue persists, seek the advice of your eye care professional. This is especially important if your eye strain is associated with headaches, pain or discomfort, double vision, or significant changes in vision.
Eye Pain (Eyes Hurt)
Whether it’s dull aching or throbbing, sharp or stabbing, eye pain is never a good sign. Eye pain is usually classified into two broad categories: ocular pain and orbital pain.
Ocular Eye Pain
Ocular pain is eye pain coming from the outer structures of the surface of the eye. Sharp ocular pain frequently accompanies conjunctivitis and other problems with the cornea (such as an infection or ulcers). Corneal abrasions and corneal ulcerations are also common causes of ocular eye pain.
Orbital Eye Pain
Orbital pain is described as a deep, dull ache behind or in the eye. This pain is often symptomatic of eye diseases. A sudden onset of severe, deep, aching orbital pain could be a sign of glaucoma. Orbital pain can sometime be a manifestation of serious eye disease such as uveitis and optic neurotis. Uveitis is an inflammation of the iris. Optic neuritis is an inflammation of your optic nerve brought about by viral and bacterial infections. It can cause vision loss. Orbital eye pain can also be triggered because of conditions that are not directly related to eyesight such as migraine and sinus problems. Eye pain can also be a signal that you’ve been abusing your eyes with too much work, reading, driving, or digital devices.
Eye pain is never a good sign. If you experience eye pain, contact an eye care professional to rule out any serious or critical eye condition that could put your sight in danger.
Eye Pressure
Eye pressure is essential to your sight. Your eye is a closed ball filled with clear jelly (vitreous humour) as well as with a transparent gelatinous fluid (aqueous humour) that continually flows within your eye. The aqueous humour is in charge of maintaining the right eye pressure (or intraocular pressure) and inflating the globe of the eye. Change in eye pressure is not to be considered normal. If intraocular pressure is too high, you run the risk of developing glaucoma, a disease that damages the optic nerve.
Glaucoma typically causes no pain and produces no symptoms. Left untreated, it can eventually affect your peripheral vision and eventually cause permanent eye damage and even blindness.
Changes in intraocular pressure may be caused by:
- Excessive or decreased aqueous production
- Inadequate or increased aqueous drainage
- Long-term use of certain medications, more specifically corticosteroids
Elevated or increased intraocular pressure can be a symptom of the following eye diseases and trauma:
- Pseudoexfoliation syndrome, a disease characterized by tiny microscopic white or grey granular flakes which are clumps of proteins within the eye
- Pigment dispersion syndrome, a form of glaucoma that happens when pigment cells slough off from the back of the iris and float around in the aqueous humour
- Corneal arcus, a common condition in which a ring of lipids builds up around the cornea
Decreased intraocular pressure is also possible and is called hypotony.
Elevated or decreased intraocular pressure is a warning signal that should not be taken lightly. If left untreated it can result in partial or total blindness in more severe cases.
Since elevated or decrease eye pressure causes no symptoms, it is important that you see an eye care professional at least every year – especially if you are over 40. An exhaustive eye exam by a qualified eye care professional will help you discover the cause and the most appropriate course of treatment to bring your intraocular pressure under control.
Eye Irritation and Inflammation - Red Eyes
Eyes can become irritated or inflamed, to the point of becoming red, when they are exposed to irritants like cigarette smoke, chlorine from a swimming pool, dust, grit, sand, etc.
Allergies to a variety of triggers such as dust and pets may also cause eye irritation and inflammation (allergic conjunctivitis).
Blepharitis (an inflammation of the eyelid follicles) and conjunctivitis (an infection of the lining of the inner eyelid) can also be behind eye itchiness and irritation.
A broken blood vessel might be the cause of eye redness. Sometimes, blood will appear underneath the clear surface of your eye when you strain, sneeze, or cough too hard (subconjunctival hemorrhage). This little hemorrhage, even though it may look impressive, is almost always harmless and will usually heal on its own within 7 days. Hyphema is another form of eye bleeding. This time blood appears between the iris and the cornea as the result of a trauma, usually because of a sharp or blunt object. The presence of a hyphema is not to be taken lightly. This type of hemorrhage can also be a consequence of many eye diseases such as herpetic kerato-uveitis (itself a risk factor for glaucoma), rubeosis iridis, and leukemia. Hyphema can also appear as a side effect of medication that alters clotting such as aspirin or vitamin K antagonists (like Coumadin).
Eye redness can also occur when other parts of the eye become inflamed, such as in episcleritis (an inflammation of the tissue that lies between the conjunctiva and the white of the eye) and uveitis (an inflammation of the pigmented middle of the three concentric layers that make up your eye), or infected, as in corneal ulcers. Eye irritation and redness should be promptly examined by your eye care professional, especially if it’s the result of a puncture or a blunt wound, as small as it is. Bleeding between the cornea and the iris is also not to be taken lightly, as it’s often associated with eye diseases that can severely affect your sight. An exhaustive eye exam by a qualified eye care professional will help you discover the source of the redness and/or bleeding and take appropriate action.
Eye Discharge
Some eye discharge, in the form of dried mucus, is not something to worry about. However, excessive discharge and crusting on the eyelids and eyelashes – especially if green or yellowish – can indicate a serious eye disease and should be promptly examined by your eye care professional. Discharge may be a manifestation of viral or bacterial conjunctivitis (“pink eye”) or keratitis (inflammation of the cornea). Some cases of blepharitis will feature some clogging of the oil glands, which can result in swollen and crusty eyelids as well as discharge. Blockage of the tear duct (dacryocystitis) can also leave you with eye discharge and crusting around the eyelids. The presence of a foreign body in the eye and corneal ulcers are two other causes of discharge. If not treated promptly, both of these eye conditions can lead to partial or complete vision loss.
An eye discharge accompanied by blurry vision, light sensitivity, or eye pain should also be considered serious and warrant an immediate visit to your eye doctor.
Watering Eyes
Tearing is a normal function of the eye. It is the way the eyes self-lubricate and defend against infection and irritation.
Watery eyes can be caused by:
- Conjunctivitis and blepharitis
- An allergic reaction to dust, mould, or animal dander
- The presence of a foreign object in the eye – sand, cigarette smoke, smog and even wind. The eyes water up to force this item out.
- A blockage in or around the eye, such as a blocked tear duct or a stye (a red lump similar to a pimple)
- Eyes may tear up during strain of overuse • A scratch or cut to part of the eye
All this being said, the most common reason for watering eyes is simply dry eyes. Although watering is not considered an emergency, contact your eye care professional immediately if it is accompanied by red eyes, excess discharge, and pain in the eye.
EYE DISEASES
Several eye diseases can affect your vision: conjunctivitis (or « pink eye »), glaucoma, cataracts, macular degeneration. This section will help you quickly identify the warning signs and symptoms of the four most common eye diseases as well as ways to prevent and treat them.
Conjunctivitis (or “Pink Eye”)
Conjunctivitis (or “Pink Eye”) is a common eye ailment where the white of the eye becomes red or pink in color. Conjunctivitis may be caused by a scratch or a small wound on the eye as well as by infections, viruses, or allergies and might be highly contagious. Even though most manifestations of conjunctivitis pose no threat, some can seriously damage your sight and require the intervention of a qualified eye care professional.
Signs Here are some of the most common symptoms of conjunctivitis:
- The white of your eye is red or pinkish
- Watering, tearing
- Itchy eyes or feeling you like have “something” caught in your eye (“foreign body sensation”)
- Clear watery discharge if the cause is from allergens. If discharge is sticky, white, or yellowish, your conjunctivitis is probably bacterial or viral and highly contagious. Eyes may be glued together upon waking up due to crusty discharge.
- Swollen lymph nodes in front of your ears and a sore throat often appear with severe bacterial conjunctivitis
- A runny nose and puffy eyes may signify you have an allergic conjunctivitis • Vision alteration and pain are NOT usual conjunctivitis symptoms. If you develop any of these symptoms, you should call your doctor immediately.
Causes
Conjunctivitis (or “Pink Eye”) may be caused by allergies, bacterial and viral infections, or an irritation. Allergic conjunctivitis is more common during spring and fall, two of the worst seasons for pollen allergies. It affects both eyes. Allergic conjunctivitis is a complication of an already existing allergic condition. Intolerance to allergens such as pollen, pet dander, dust, mold, and other substances will trigger allergic conjunctivitis.
- Giant papillary conjunctivitis (GPC):
- Giant papillary conjunctivitis is a type of allergic conjunctivitis caused by a foreign body that irritates the eye. Most commonly, this reaction is cause by contact lenses. It is estimated that around 21 % of lens wearer will experience GPC. This condition mostly affects those who wear soft contact lenses.
- Bacterial conjunctivitis:
- Bacterial conjunctivitis is one of the most commonly encountered eye diseases. This type of conjunctivitis usually causes a red eye with a lot of puss. It is self-limiting in the sense that most benign cases will heal in about 7 to 10 days with the right care. Bacterial conjunctivitis is more common in children than in adults.
- Viral conjunctivitis:
- The most common cause of viral conjunctivitis is the same virus that causes the common cold. For this reason, it can be associated with colds or with symptoms of a respiratory infection, such as a sore throat. Viral conjunctivitis usually produces a watery discharge and is very contagious. It is also self-limiting in the sense that most benign cases will heal in about 7 to 10 days with the right care.
- Irritations:
- Irritation resulting from a foreign object in your eyes (or irritating substance such as a chemical) is also associated with mild conjunctivitis. It will generally affect only one of your eyes and will clear up in about one day with the right care.
Remedies and Medication
- Allergic Conjunctivitis Treatments:
- Your eye care professional might prescribe one of the many allergy eye drops available on the market. These include medication to control the symptoms of allergic reactions such as antihistamine, anti-inflammatory, decongestant, mast cell stabilizers, and multiple action drops.
- Bacterial Conjunctivitis:
- Treatments Antibiotic and anti-inflammatory eye drops will usually be prescribed to treat bacterial conjunctivitis. An antibiotic eye ointment will usually be recommended for younger kids as it is easier to administer. Vision can be blurry for up to 20 minutes after application.
- Viral Conjunctivitis Treatments:
- Eye care professionals will not prescribe any drugs for viral conjunctivitis. The preferred treatment for most mild case will be to let this eye disease run its course. Viral conjunctivitis will usually infect one eye and then the other within a couple of days. Antiviral drops and medication might be prescribed in rare cases if it is determined that your viral conjunctivitis is caused by the herpes virus.
Surgery
Surgical intervention is required only to correct causes that brought about the conjunctivitis, such as lachrymal duct obstruction and sinusitis.
Prevention
The best prevention for allergic conjunctivitis is simply to avoid the allergen you are sensitive to. Other options include:
- Desensitization to specific allergens
- Prevention of Bacterial and Viral Conjunctivitis
- Hand washing and good hygiene techniques will generally help you avoid most conjunctivitis-causing bacteria
- You should also avoid touching or rubbing your eyes and wash any discharge around the eyes several times a day. Do not share articles like towels, blankets, and pillowcases
Even though most manifestations of conjunctivitis pose no threat, some can seriously damage your sight and require the intervention of a qualified eye care professional.
Glaucoma
Glaucoma develops when the intraocular pressure of your eye is too high. Glaucoma typically causes no pain and produces no symptoms. Left untreated, it can eventually affect your peripheral vision and eventually cause permanent eye damage and even blindness.
Symptoms and Signs
Glaucoma is often called a “silent disease” as its most common form (open-angle glaucoma) involves no warning signs or symptoms whatsoever. Some people might notice a very slow loss of side vision over time (“tunnel vision”). The acute form of glaucoma, angle-closure glaucoma, presents a serious health risk. Intraocular pressure will rise very quickly to dangerous levels, often in a matter of hours. In that case, the patient will feel intense pain with redness of the eye. Nausea and vomiting may be present. Vision quickly becomes cloudy, sometime with rainbow-like halos appearing around bright lights. Angle-closure glaucoma is a medical urgency requiring immediate attention as irreparable damage can be done to your sight in a matter of hours.
Causes
Both types of glaucoma are caused by an increase of intraocular pressure that eventually irreversibly damages your optical nerve and leads to a loss of your visual field. The increased intraocular pressure happens gradually in open-angle glaucoma. This pressure on the optic nerve eventually causes blind spots in your vision. This slow build-up explains why patients usually do not feel the slow increase of intraocular pressure. Angle-closure glaucoma is something else entirely. It involves a sudden build-up of aqueous humour that does not flow out of the eye properly, causing a severe and sudden rise in intraocular pressure.
Both types of glaucoma can occur due to:
- Use of corticosteroids
- Eye drops that dilate your eyes
- Some eye diseases
- Diabetes
- Previous eye injury
Remedies and Medication
A variety of options can be used in the treatment of glaucoma, including eye drops, laser therapy, and surgery. Eye drops are often the first choice of treatment to reduce intraocular pressure and prevent optic nerve damage. Glaucoma can be controlled—provided it is detected early—if the patient takes his medicine every day and sees their eye care professional regularly.
Surgery
In cases where eye drops and pills are of limited efficacy, laser trabeculoplasty can be recommended as a treatment procedure to lower intraocular pressure. Laser trabeculoplasty involves the use of a high-intensity beam of light aimed through the lens to treat the drainage angle of the eye. It’s usually done in your eye care professional’s office. Conventional surgery can also be recommended in some cases.
Prevention
Currently, regular eye exams constitute the best form of prevention against significant glaucoma damage.
Macular Degeneration Treatment
Macular degeneration is a chronic and progressive age-related eye disease that affects the center of your retina (the macula). Macular degeneration leads to loss of your central vision, which means everything you see directly in front of you. This eye disease can prevent you from doing things you take for granted such as driving, reading or watch TV. In Canada, macular degeneration is the leading cause of legal blindness for people over the age of 50. A hereditary form, named Stargardt macular degeneration, can affect children and teens. The non-hereditary macular degeneration occurs in "dry" and "wet" forms.
Dry macular degeneration is also known as atrophic macular degeneration. This more frequent type of macular degeneration involves the slow and progressive death of critical cells in the macula. This process eventually creates “blind spots” in your vision. As critical to your eyesight as it is, dry macular degeneration is considered less severe than wet macular degeneration. Wet macular degeneration is also known as exsudative macular degeneration. Less frequent than the “dry” form, this type of macular degeneration always starts out as cases of dry macular degeneration. The exsudative type of macular degeneration is characterized by the appearance of new veins under the retina that often break and cause a scar on its central part, the macula.
If you notice any change in your central vision, you should immediately consult a qualified eye care professional.
Symptoms and signs
Many people suffering from macular degeneration will display absolutely no symptoms in the early stage of the disease. As the disease progresses, more painless symptoms appear such as:
- Requiring more light to read or execute precision work
- Central vision becomes blurred
- Difficulty adjusting between dark and light conditions
- Colors appear faded and are more difficult to tell apart
- Straight lines are distorted when seen from close or far away
- Advanced stages may feature a little dark spot in the middle of your field of vision
- Facial features are difficult to recognize • Visual hallucinations such as geometric shapes, animals, distorted faces, etc.
Causes
Macular degeneration has no known cause. Age seems to be involved in its development at some level. Other suspected risks include:
- Heredity: If you have a family history of macular degeneration, you are more likely to suffer from this eye disease.
- Smoking: Studies have shown that smokers are 2 to 3 times more likely to develop macular degeneration than non-smokers.
- Hypertension and dietary habits.
- Previous eye inflammation: Research has found a relation between C-reactive protein rates (an inflammation marker) and macular degeneration.
- Previous vascular episodes: People with previous vascular troubles are more at risk of developing macular degeneration.
Medication
- Atrophic (Dry) macular degeneration:
- The dry form of macular degeneration has no known cure. Recent studies have however discovered that some antioxidant vitamins can reduce its progression. However, these elements have no preventive value per se. Since the publication of the AREDS study in 2001 by the National Eye Institute (NEI) many eye care professionals have began to prescribe a special antioxidant supplement that patients take daily. The formula is sold under different brand names such as ICaps®, Macuvision®, Ocuvite PreserVision®, Super Vision® and Vitalux Areds®. These nutrients are also found in a healthy diet that includes a variety of fruits and vegetables, unsaturated fat, whole grains, and fish rich in Omega-3 fatty acids.
- Exudative (Wet) macular degeneration:
- Your eye care professional can inject drugs directly into your eye to stop the growth of new blood vessels. The most widely used medications are Bevacizumab (Avastin), Ranibizumab (Lucentis), Pegaptanib (Macugen) or Aflibercept (Eylea). Other methods are also available to treat abnormal blood vessels such as photodynamic therapy (a light-activated drug that eliminates the abnormal blood vessels) and photocoagulation (use of a laser to destroy abnormal blood vessels).
Surgery
A few experimental surgical options were investigated to eliminate or remove abnormal blood vessels like submacular surgery and retinal translocation. So far, retinal translocation has shown promising results in clinical trials. This experimental procedure involves rotating the macula away from the abnormal blood vessels to a healthy area of the retina.
Prevention
Even though some risk factors cannot be controlled, there are many lifestyle adjustments you can make to reduce your risk of developing macular degeneration.
- Manage your other medical conditions like diabetes, high blood pressure etc. Stick closely to your treatment plan
- Quit smoking and cut down alcohol
- Adopt a healthy diet. A diet rich in vitamins and mineral has been linked with a reduced risk of developing macular degeneration
- Be physically active
- Protect your eyes from UV rays
- Have your eyes regularly checked up by a qualified eye care professional
If you are over 40, regular check-ups with a qualified eye care professional can help detect early stage macular degeneration.
Cataract Surgery - Cataracts Removal
Cataracts are a protein build-up in the lens that makes it cloudy and impair vision. Symptoms include cloudy or blurry vision and an increased sensitivity to glare. Cataracts affect more than 1 in 5 Canadians over age 65. This figure gets even more alarming with 1 in 3 Canadians over 75. In total, 2.5 million Canadians have cataracts. In fact, cataracts are the third leading cause of blindness in Canada after macular degeneration and glaucoma. If you are over the age of 40, a check-up with a qualified eye care professional every two year constitutes the best way to detect cataracts.
Symptoms and Signs
Even though they are painless, there are still some signs and symptoms that may suggest you’re suffering from cataracts:
- Cloudy or blurry vision, glare and decreased night vision
- Loss of contrast sensitivity: shadows and colours are less vivid
- Veiled vision, objects seems to be behind a white veil
- “Seeing double” (diplopia): perceiving two images of a single object at the same time
- Frequent change in eyeglass or contact lenses prescription – myopia (nearsightedness) tends to get worse in the early stages of cataract formation
Causes
Even though cataracts are often an age-related condition, several other causes are suspected, including:
- Eye trauma, or as a consequence of injuries involving puncture and blunt wounds to the eye
- Ultraviolet light (UV-B) and other types of radiation that alter the structure of the lens
- Heredity
- Diabetes
- Some skin diseases such as eczema and atopic dermatitis
- Hypertension
- Smoking
- Prolonged use of corticosteroid medication
Remedies and Medication
Even though some alternative health practitioners may recommend natural cure (homeopathic compounds, bentonite clay, or the plant cineraria maratima) or dietary means (beta-carotene, vitamin C, and vitamin E supplements) to treat cataracts, the only scientifically proven method of stopping the progression of this eye disease and reversing some of its effects remains surgery.
Prevention
There are no proven ways to prevent cataracts from forming. Eye care professionals can however recommend some lifestyle adjustments that will help keep your sight healthy and may attenuate some known risk factors:
- Wear sunglasses: UV rays from the sun may contribute to the development of cataracts
- If you have diabetes, stick closely to your treatment plan
- Quit smoking and cut down alcoho
- Eat plenty of fruits and vegetables: A diet rich in vitamins and mineral has been linked with a reduced risk of developing cataracts
- Regular eye exams with a qualified eye care professional: If you are over 40, regular check-ups with a qualified eye care professional can help detect cataracts and other eye problems at their earliest stages
If you are over the age of 40, a check-up with a qualified eye care professional every two years constitute the best way to detect cataracts.
Emergency Eye Symptoms
Some symptoms require immediate medical attention such as:
- Temporary or continued partial blindness in one or both eyes
- Temporary or continued double vision
- Vision change that seems to be associated with a medication you take
- Blind spots, halos around lights, or areas of distorted vision suddenly appear
- Eye pain, especially if there is some eye redness. A red, painful eye is a medical emergency
- You feel like a shade is being pulled down or a curtain pulled across your vision
Make an appointment as soon as possible with an eye care provider if you experience any of the following:
- Trouble seeing objects to either side
- Difficulty seeing at night or when reading
- Gradual loss of the sharpness of your vision
- Difficulty distinguishing colours
- Blurred vision when trying to view objects near or far